Anterior Cruciate Ligament (ACL) Reconstruction
The goal of treatment for an Anterior Cruciate Ligament (ACL) tear is to decrease pain and restore function to the knee. Because of the poor blood supply to the ACL, very rarely do they heal on their own. However, not all ACL tears need to be treated with surgery. The treatment recommended by your doctor will depend on your age as well as the activities and sports you enjoy doing. Also, the presence of other injuries within the knee can affect the prognosis as well as speed of recovery.
Graft Choice
As mentioned above, there are different graft options available for ACL reconstruction. There are pros and cons to each; which type we recommend will depend on your age, activity level, and associated injuries.
Autografts are tissues from your own body. There are two main autograft options:
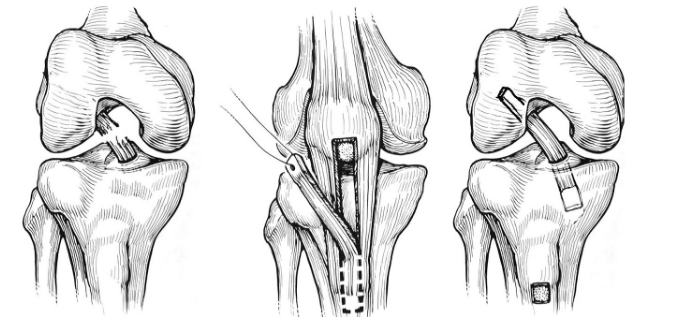
- Patellar tendon grafts use the middle 1/3 of the patellar tendon with bone pieces on each end— one from the patella and one from the tibia. The bone ends are fixed in the tunnels with large screws, ultimately with bone to bone healing, which is strong and reliable. Patellar tendon grafts are often used for young active individuals (16-23 years old) that play sports like football, soccer, and lacrosse. The downside to using this graft is that it can be more painful right after surgery than other graft choices. There is also an increased risk of having pain or cartilage wear behind the kneecap. It is estimated that 20% of patients experience this, although it has lessened with newer rehabilitation techniques. In addition, the rehabilitation with a patellar tendon graft is more intense and takes more effort than for other graft types.
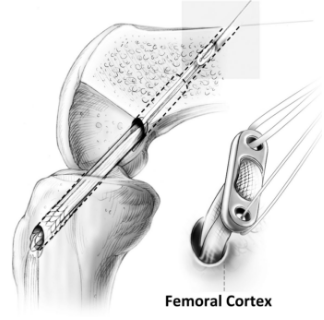
- Hamstring grafts use two of the five hamstring tendons from the inside of the knee. These two tendons are sewn together to create a substantial graft that behaves much like the native ACL. This graft can be fixed to the bone tunnels with a variety of methods. Patients seem to recover a bit quicker because there is less pain in the front of the knee. There is little to no noticeable loss in knee flexion (hamstring) strength, and it appears that most of the harvested tendon regenerates or attaches itself to the other hamstring muscles. The downside to using the hamstring tendon graft is that it seems to loosen slightly more than the patellar tendon graft. This does not seem to be a problem for most athletes, particularly older or recreational athletes or those playing non-contact sports.
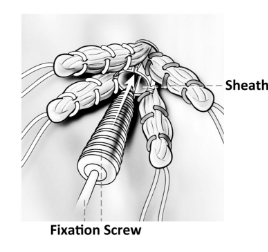
- Allografts are donated (cadaver) tissues. There are a few different kinds that are used routinely: patellar tendon, Achilles tendon, and soft tissue. The strength of these is very similar to the native ACL. The fixation methods vary depending on the type of tendon used, but in general all seem to work well.
Allograft is an attractive option because we do not remove anything else from your knee. Because of this, the early post-operative period is less painful and patients tend to be on their feet more quickly. In addition, allograft is often the best or only option for individuals who require multi-ligament knee surgery or revision surgery.
As soon as the allograft tissue is placed into the knee, it begins a rebuilding and remodeling process similar to the other graft types. The collagen in the allograft acts as a scaffold for your cells so that over time, the allograft tissue becomes part of you. Thus, the healing and remodeling process takes a bit longer with an allograft, even though you feel better more quickly. This means that we slow down your rehabilitation to protect the graft while it heals. This also generally means a longer time before returning to sports.
The downside of using allograft tissue is that it is not from your own body. As a result, there is a small risk of viral and bacterial disease transmission. The risk of contracting HIV or hepatitis from a graft is estimated to range from 1 in 600,000 to 1 in 1.6 million. Current allograft screening and preparation techniques are very rigorous. As such, in the last twenty years, the risk of bacterial and or viral infection has been reduced significantly.
Postoperative Timeline
Your rehabilitation and return to activity depend on a number of factors including graft type, associated injuries and their treatments, and your surgeon’s preferences. This is only a rough guideline of what to expect, and you should discuss the specifics of returning to activity with your surgeon.
- Crutches for 2-3 weeks post operatively. These are stopped when your quadriceps muscle starts working again.
- Physical therapy 2-3 times per week, with an additional home exercise program.
- Your surgeon may want you to use a brace to protect the knee after surgery. He or she may also recommend a functional brace for sports and activities for a year or more after surgery.
- Return to team sports (assuming appropriate progression with therapy) at 6-12 months, depending on the graft type and sport.
- When you return to work depends on your job:
School, sedentary or desk work— 1-2 weeks
Light duty (more walking or standing) — 3-6 weeks
Heavy labor— 3-6 months
This surgery is complex and there are some specific complications that can occur:
- Post-operative fluid in the knee (can require drainage in the office)
- Continued pain and stiffness due to scarring in the knee or around the graft
- Need for re-operation to address a new meniscal tear or scarring
- Re-tear or progressive loosening of the graft
- New meniscus tear or articular cartilage injury
- Development or progression of knee arthritis
A more general complication of surgery can also occur and would include:
- Deep venous thrombosis (aka “blood clot” or DVT)
- Infection (all patients receive antibiotics at the time of surgery to decrease this risk)
- Nerve injury (associated with numbness, weakness, or paralysis)
- Vascular injury or compartment syndrome
- Complications associated with the anesthesia
